Revenue cycle management (RCM) creates a seamless system that minimizes inefficiencies and maximizes revenue throughout different companies. According to the Healthcare Financial Management Association (HFMA), effective RCM can improve collections by up to 20% while reducing operational costs by 15% or more.
Now that you’re looking at it, you’re probably thinking woaaah that’s a big number. Which it is indeed. But now you want to know the secret, the answer to the question of – How can an organization improve its revenue cycle management?
No worries, we won’t hide the answer from you any longer, let’s begin with the 8 ways in which the organizations are improving their RCMs.
They’re Automating Their Processes
Automation is transforming revenue cycle management, helping organizations streamline tasks, reduce errors, and improve efficiency. A study by Black Book Market Research found that 85% of healthcare providers who implemented RCM automation saw an increase in productivity and a reduction in claim denials.
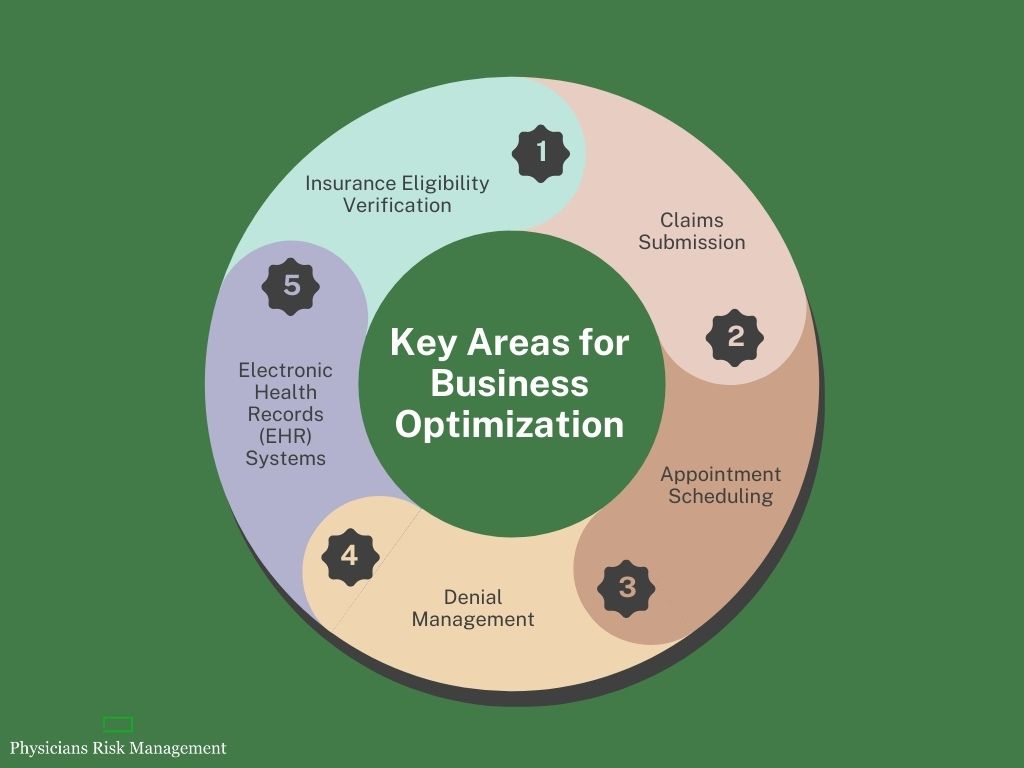
Key Automation Areas:
- Insurance Eligibility Verification: Tools that verify patient insurance in real time can prevent delays caused by incorrect or incomplete information.
- Claims Submission: Automatic claim generators expedite the submission process and ensure accuracy, reducing denials. For example, automated claims processing has been shown to cut errors by 50%, according to industry reports.
- Appointment Scheduling: Automated systems allow patients to book, reschedule, and receive reminders, enhancing the overall experience.
- Denial Management: Automated claim tracking systems identify and categorize denied claims for faster resolution.
- Electronic Health Records (EHR) Systems: Integrating EHR with practice management software creates a unified workflow, ensuring smooth data transfer.
Organisations can greatly enhance their revenue cycles by implementing workflow automation solutions such as practice management software and utilising the card-on-file technique to expedite payment processing.
They’re Utilizing Data and Analytics
Data is the backbone of modern RCM strategies. Healthcare providers may identify inefficiencies and put data-driven solutions into place with the help of the appropriate analytics tools. According to McKinsey, data-driven healthcare organizations are 23% more likely to outperform their peers in financial performance.
Key Benefits of Analytics:
- Real-Time Insights: Advanced analytics tools provide a snapshot of current performance, enabling quick decision-making.
- DNFB Analytics Applications: These tools identify revenue held up in claims not yet billed, speeding up cash flow.
- KPI Tracking: Monitoring metrics like claim denial rates, collection rates, and days in accounts receivable ensures continuous improvement.
- Periodic Audits and Assessments: Regularly reviewing financial data helps pinpoint trends and areas needing improvement.
Platforms like the Health Catalyst Data Operating System (DOS™) provide powerful analytics capabilities to optimize RCM processes. Using these tools, organizations can transition to a data-driven revenue cycle that prioritizes performance.
They’re Mastering Denial Management
A systematic approach to denial management can save time and recover lost revenue. According to the American Medical Association (AMA), denial rates in healthcare can range from 5% to 10%, representing millions of dollars in potential losses annually for larger organizations.
Strategies for Effective Denial Management:
- Root Cause Analysis: Identify why claims are denied and implement prevention plans.
- Appeal Process: Streamline appeals to ensure timely resolution of denied claims.
- Automated Tracking: Use analytics solutions to monitor and manage denied claims efficiently.
- Staff Training: Equip your team with the knowledge to handle denials effectively.
- Regular Audits: Routine reviews help uncover patterns and refine strategies.
A robust denial management plan reduces denial management challenges, and also improves payer negotiations and patient satisfaction.
They’re Enhancing Appointment Scheduling
Missed appointments and inefficient scheduling can impact both patient care and revenue.
Improving this aspect of the revenue cycle requires thoughtful strategies and modern tools. A study by the Medical Group Management Association (MGMA) revealed that practices lose an average of $200 per missed appointment.
Best Practices:
- Online Scheduling Tools: Allow patients to book and manage appointments digitally.
- Automated Patient Reminders: Use text or email notifications to reduce no-shows.
- Flexible Hours: Accommodating patients’ schedules can increase attendance.
- Analyzing Appointment Trends: Use data to identify peak times and adjust schedules accordingly.
These improvements enhance the patient experience, but it also strengthens the financial health of the organization by minimizing wait times and optimizing resources.
Or You can Outsource RCM Services
For some organizations, outsourcing revenue cycle management services is a practical solution. Specialized firms bring expertise, advanced tools, and scalability to the table.
The global outsourced medical billing market is projected to grow to $19.7 billion by 2027, according to Grand View Research, underscoring its importance in modern healthcare.
Benefits of Outsourcing:
- Focus on Core Services: Outsourcing frees up internal resources for patient care.
- Customized RCM Solutions: Tailored approaches ensure that the organization’s unique needs are met.
- Improved Efficiency: Experts handle tasks like insurance verification and clinical documentation, reducing errors.
- Cost Savings: Outsourcing often reduces overhead costs associated with in-house RCM.
Partnering with a medical billing company or using revenue cycle management software can drive better outcomes and allow healthcare providers to concentrate on what they do best—delivering care.
Simplifying Patient Payment Processes
Clear and efficient payment processes are vital for improving cash flow and patient satisfaction. Upfront collections and flexible options can make a significant difference.
According to InstaMed’s Trends in Healthcare Payments Report, 70% of patients prefer to pay their medical bills online, highlighting the importance of digital payment options.
Key Strategies:
- Credit-Card-on-File Services: Simplify recurring payments and reduce administrative tasks.
- Contactless Payment Methods: Offer convenience through mobile wallets and online bill pay.
- Propensity-to-Pay Predictive Models: Use analytics to identify patients likely to pay and tailor approaches accordingly.
- Upfront Collections: Collecting payments during registration or at the time of service minimizes outstanding balances.
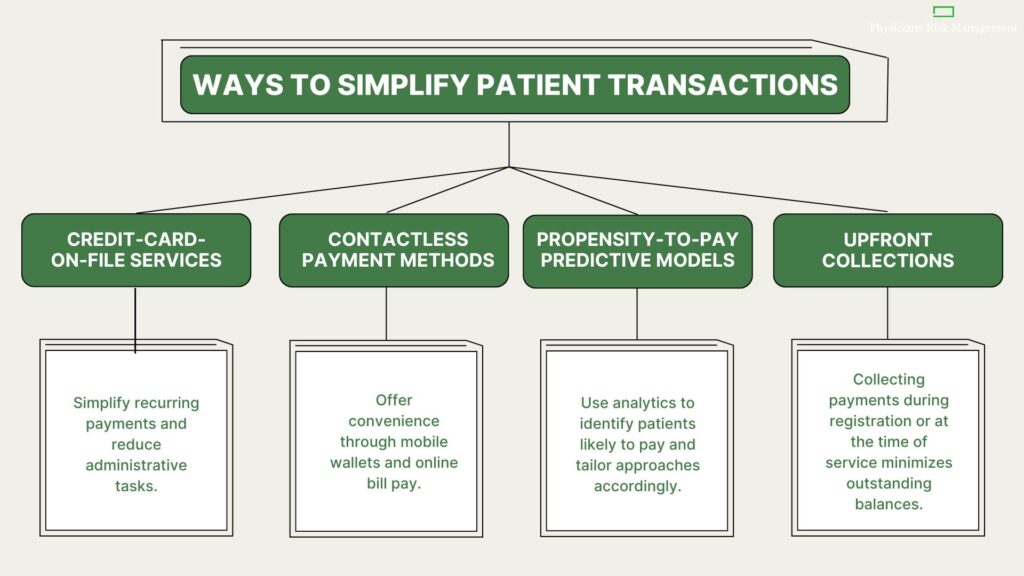
Healthcare providers can improve the whole billing and payment collection process and lessen billing difficulties by putting these ideas into practice.
Ensuring Quality Billing and Coding Practices
Accurate billing and coding are the foundation of successful revenue cycle management. Errors in these areas can lead to denials, delays, and revenue loss.
The Workgroup for Electronic Data Interchange (WEDI) estimates that coding errors contribute to 42% of denied claims.
Best Practices:
- Advanced Coding Software: Tools that update with the latest medical coding changes ensure compliance and accuracy.
- Billing Technology: Streamlined technology minimizes errors and optimizes claims submission.
- Staff Training: Regular updates on coding practices keep your team informed.
Maintaining high standards in these areas reduces claim denials and ensures that revenue flows smoothly.
Investing in Staff Training and Development
A well-trained team is important for efficient RCM. Staff investment not only improves performance but also boosts morale and reduces turnover. According to a report by Deloitte, 72% of healthcare executives believe that investing in staff training significantly enhances operational efficiency.
Training Focus Areas:
- Claims Procedures: Teach staff how to handle claims effectively.
- Coding Practices: Ensure compliance with the latest billing codes.
- Patient Payment Collection: Train on strategies to improve upfront collections.
- Technology Utilization: Equip teams to use RCM system software and other tools efficiently.
Investing in educational resources and developing a revenue cycle management action plan enhances your team’s capabilities and sets the stage for long-term success.
Now We Know How Can an Organization Improve Its Revenue Cycle Management, But How Can We Apply It?
Improving revenue cycle management requires a combination of automation, data-driven decision-making, efficient denial management, optimized scheduling, outsourcing, and staff training.
Physician Risk Management knows the complexities of managing revenue cycles effectively. That’s why our experts are here to make your RCM experience efficient, productive, and results-driven.
Partner with us to identify gaps, implement tailored strategies, and elevate your revenue cycle management. Let us take care of RCM and other paperwork so you can focus on delivering exceptional care to your patients.
Together, we can achieve sustainable financial success and a better experience for everyone involved.